What is Vascular Dementia?

Share this Infographic Image On Your Site
What is Vascular Dementia?
Vascular dementia is a type of dementia caused by reduced blood flow to the brain. While most people think of Alzheimer’s disease when they hear the word “dementia,” vascular dementia is the second most common type of dementia, behind Alzheimer’s, and causes similar symptoms. In fact, the two often go hand-in-hand.
Mixed dementia is a type of dementia that includes Alzheimer’s and vascular dementia. Only 5-10% of vascular dementia cases are only vascular dementia. Most cases are mixed dementia.
Multi-infarct dementia, also known as vascular cognitive impairment, is a type of vascular dementia caused by a series of blockages that affect blood flow to a certain area of the brain. These blockages often go undetected until they cause symptoms that affect cognitive function.
What causes vascular dementia?
Restricted blood flow to the brain is ultimately what causes vascular dementia, and a number of factors can cause restricted blood flow, including:
Genetics can predispose someone to vascular dementia. CADASIL (cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy) is a genetic disorder that affects blood vessels in the brain, causing migraines, seizures, severe depression and, ultimately, vascular dementia.
What are the symptoms of vascular dementia?
Symptoms of vascular dementia vary based on which part of the brain is affected.
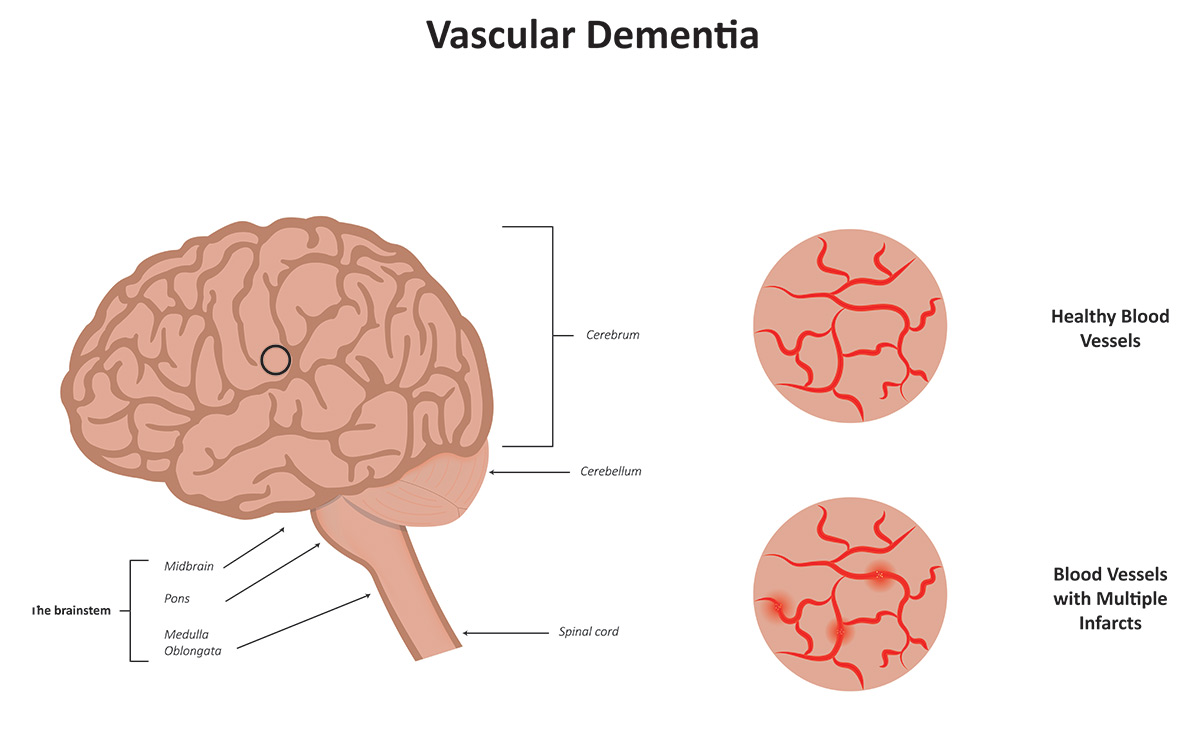
Vascular dementia caused by a major stroke can damage one side of the brain where blood supply was cut off. People with this type of vascular dementia may experience the following symptoms:
Multi-infarct dementia is caused by a series of mini-strokes that result in dead brain tissue in various areas of the brain, known as an infarct. If there is an infarct in the hippocampus, memory will be affected. If there’s an infarct in the frontal lobe, executive function will be affected.
Subcortical vascular dementia is a type of vascular dementia that affects the white matter in the brain beneath the cortex, which is responsible for sending signals in the brain. Damage to white matter results in slowed thinking and difficulty with executive functioning.
Other symptoms of vascular dementia include:
Who is at risk for vascular dementia?
Because vascular dementia is caused by restricted blood flow to the brain, anything that affects heart health can put someone at higher risk for developing vascular dementia, including:
Aging also puts you at higher risk. From age 65 to 90, the risk for developing vascular dementia greatly increases.
Can you prevent vascular dementia?
While there is no sure-fire way to ensure you will never get vascular dementia, keeping your heart healthy is the best thing you can do to lower your risk of developing vascular dementia. You can do this by:
How is vascular dementia treated?
There is no cure for vascular dementia, but symptoms can be alleviated, and the progression of the disease can be slowed through activities and procedures that improve blood flow to the brain, such as:
How is vascular dementia diagnosed?
If you suspect you or a loved one is showing signs of vascular dementia, call your doctor immediately. He or she will probably refer you to a neurologist who can offer a proper exam and diagnosis.
Vascular dementia can be detected through magnetic resonance imagining (MRI), computed tomography (CT scan), or through a PET scan. A neurologist can also administer a neuropsychological assessment to determine what type of dementia you might have. You may also receive a neuropsychiatric evaluation to rule out any mental conditions that might be mimicking vascular dementia.
As the second most common type of dementia, know you are not alone if you receive a diagnosis. Vascular dementia is becoming more common and is expected to become even more common in years to come as people live longer with the types of health risks that cause vascular dementia. Talk to your doctor, get an assessment made and establish the best plan of care that will ensure you live the best life you can with vascular dementia.