How Fast Does Alzheimer’s Progress?
A serious diagnosis always raises serious questions.
What exactly does my diagnosis mean for me?
What will the disease look like?
How will it progress?
How quickly will it progress?
What is my life expectancy?
We want exact answers to our questions. A life-threatening diagnosis leaves us feeling out of control, confused and anxious. We think if we can know exactly what will happen, we will feel better.
While this is sometimes the case, doctors often can’t answer these specific questions. Every person is different. Everyone has a different health history, gene set, and environmental factors that will make their disease look and feel different.
This is especially true for Alzheimer’s disease.
One of the most common questions to arise after an Alzheimer’s diagnosis is How fast will my Alzheimer’s progress?
While doctors can make estimates based on various factors, the progression of the disease solely depends on the individual. The average life expectancy for someone with Alzheimer’s is eight to 12 years from the time of diagnosis, though people have lived up to 26 years after their diagnosis, especially if they are diagnosed early.
Because of this, knowing exactly how quickly the disease will progress can be difficult to estimate. However, understanding the factors at play can be helpful.
We’ll get into some of these factors below, but first, it’s helpful to understand how the disease progresses in most people.
Alzheimer’s can be broken down into five, sequential stages.
The 5 stages of Alzheimer’s disease
1. Preclinical Alzheimer’s disease

This stage begins before symptoms of Alzheimer’s, such as memory loss or moodiness, appear. With advanced research, we now know that Alzheimer’s can appear in the brain long before the disease is noticeable to you or others.
Genetic testing, biomarkers, neuroimaging and blood tests can all indicate whether or not someone has Alzheimer’s disease at this stage.
2. Mild cognitive impairment due to Alzheimer’s disease

The Mayo Clinic defines mild cognitive impairment (MCI) as “the stage between the expected cognitive decline of normal aging and the more serious decline of dementia.”[i]
MCI can be caused by Alzheimer’s disease or other conditions such as nutritional deficiencies, autoimmune disease, metabolic imbalance, a brain tumor and more. MCI typically causes issues with thinking, reading, learning, remembering, reasoning and attention span, but it won’t interfere with daily tasks and activities.
Testing can be done to determine if MCI is caused by Alzheimer’s or another condition.
3. Mild dementia due to Alzheimer’s disease

Mild dementia due to Alzheimer’s disease is the stage when Alzheimer’s is most commonly diagnosed because this is typically the stage when symptoms become evident to family members and doctors.
Symptoms of mild dementia due to Alzheimer’s disease include:
- Short-term memory loss: difficulty remembering recent events or information
- Poor judgment: making poor decisions due to a loss of sound judgment and reasoning skills
- Difficulty with problem-solving or completing tasks: an inability to do complex tasks such as balancing a checkbook and an inability to follow through with daily tasks after they are started
- Misplacing items: misplacing valuable items more frequently or not being able to remember where they are
- Change in personality: withdrawing in social gatherings or feeling angry or irritable more often
- Getting lost: frequently not being able to find once-familiar locations
These symptoms indicate that memory loss and other symptoms have begun to interfere with daily life, making the disease much more prominent and noticeable.
4. Moderate dementia due to Alzheimer’s disease

At this stage of Alzheimer’s, the symptoms that began in the mild dementia stage grow more severe. Memory loss and confusion increase. Basic details about your life such as your birthday may become difficult to remember. Personality and behavior changes are more evident at this stage. Many grow suspicious of their caretakers and loved ones or think they are seeing or hearing things that aren’t there.
At this stage, many may need help with activities of daily life (ADLs), such as going to the bathroom, changing clothes and eating.
5. Severe dementia due to Alzheimer’s disease

Throughout every stage of Alzheimer’s disease neurons in the brain are deteriorating, shrinking the brain. During the final stage of Alzheimer’s, the disease has affected every area of the brain needed for daily functioning, which is why the disease is fatal. This causes a patient to not be able to communicate coherently, to need assistance with all ADLs and not be able to physically move or sit up on his or her own. Eventually, someone with severe dementia due to Alzheimer’s will lose the ability to swallow or control their bowels.
Factors that determine how fast Alzheimer’s will progress
1. Age

More research needs to be done to conclude if this is always the case, but there is evidence to support that if you are diagnosed with Alzheimer’s before age 65, known as early-onset Alzheimer’s, the disease is likely to progress more quickly than if you are diagnosed over the age of 65.
This could be due to the fact that early-onset Alzheimer’s is largely associated with genetics while late-onset Alzheimer’s can be caused by a number of factors, so these two types of Alzheimer’s may have pathological differences that cause one to progress more quickly than the other.
2. Preexisting health conditions

If someone already has heart disease, diabetes, or high blood pressure at the time of their diagnosis, Alzheimer’s may progress more quickly, especially if these conditions have not been managed well. A healthy heart is essential for a healthy brain, and an unhealthy heart can do a lot of damage to the brain, especially if you have Alzheimer’s.
3. Delirium
Delirium is a condition that begins suddenly in someone who may already have dementia. Delirium causes you to feel confused and can be very distressing. Bouts of delirium can cause Alzheimer’s disease to progress more quickly.
4. Stroke
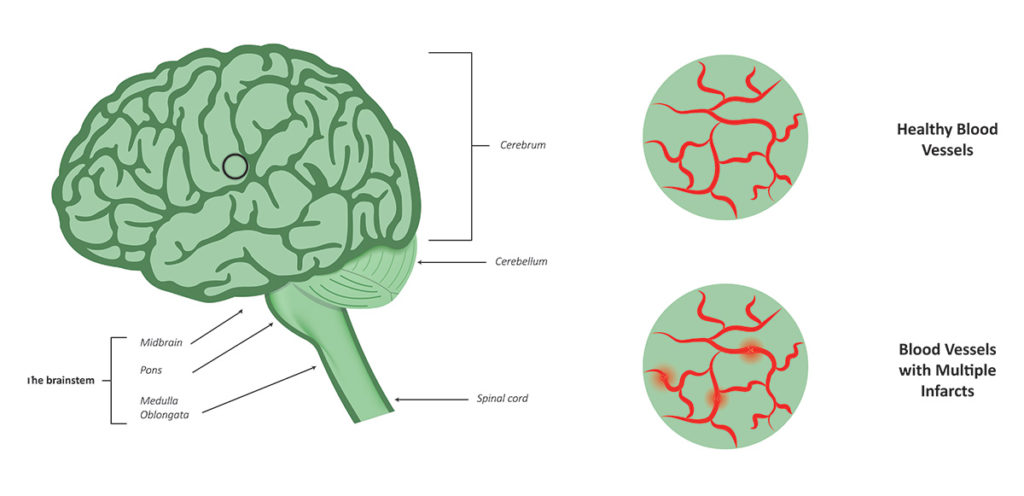
Those with vascular dementia (a type of dementia associated with decreased blood flow to the brain that almost always accompanies Alzheimer’s disease) are at higher risk for stroke. (A previous history of strokes may be the cause of their vascular dementia.) Having a stroke when you already have Alzheimer’s disease can cause the disease to progress more rapidly because strokes cause further damage to the brain.
If you’ve been diagnosed with Alzheimer’s disease, talk to your doctor about the prognosis. While doctors can’t make an exact estimate on the progression your disease will take, they can provide guidance based on your genetics, health and lifestyle. You may not get all the answers you want, but you can establish a plan of care that makes you feel safe, eases your anxiety, and ensures you will stay as healthy as possible for as long as possible.
[i] Mayo Clinic, Understanding Alzheimer’s: Your Guide to Brain Health, p.22.
Share this Infographic Image On Your Site
<p><strong>Please include attribution to https://baderhouse.com/ with this graphic.</strong><br /><br /><a href='https://baderhouse.com/how-long-can-you-live-with-dementia/'><img src='https://baderhouse.com/wp-content/uploads/2022/10/baderhouse_can-you-live-with-dementia-infographic.jpg' alt='How Long Can You Life with Dementia?' width='1200px' /></a></p>