What is the connection between dementia and depression?

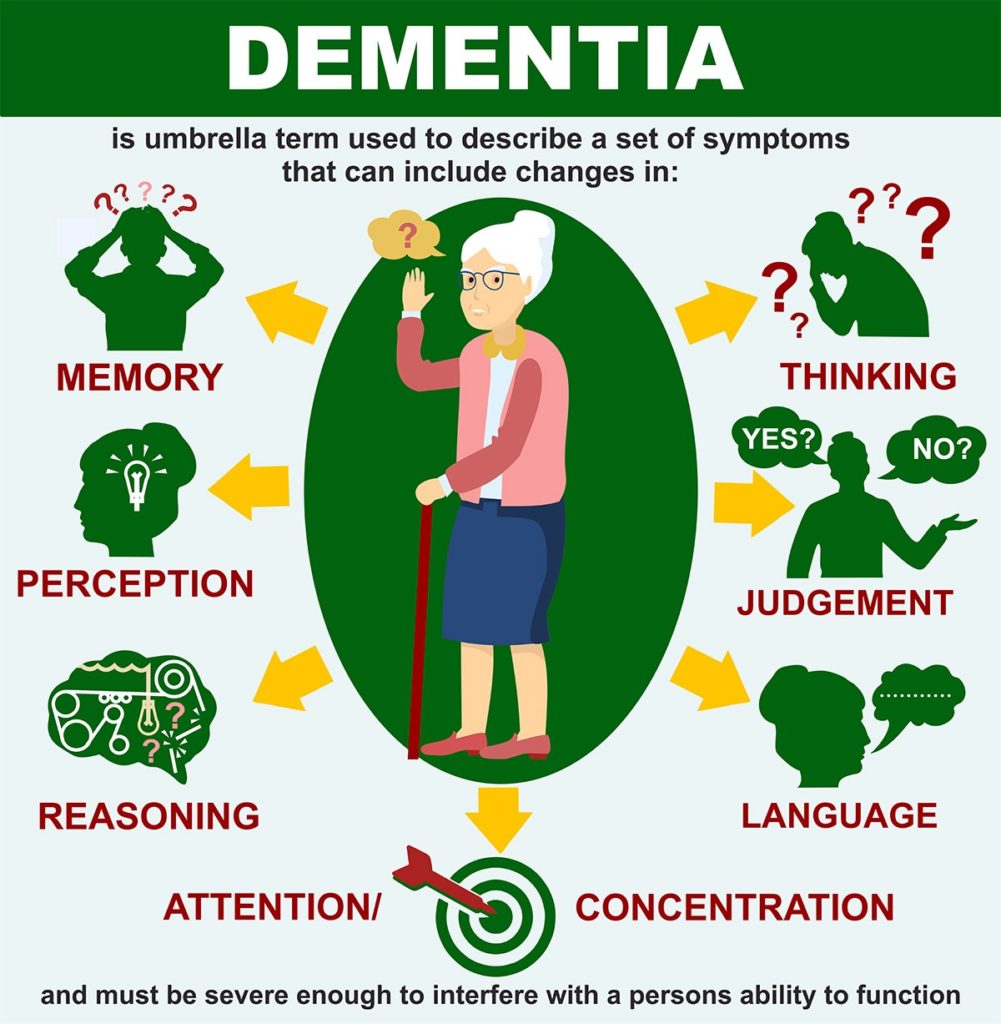
Symptoms of depression and symptoms of dementia can appear similar in older adults. Withdrawal, difficulty with memory, and mood swings can be signs of depression or dementia or both.
This makes self-diagnosis or trying to diagnose your family member incredibly difficult. Do they have a mood disorder or are they suffering from cognitive decline? Only a doctor can tell you for sure, but understanding the connection between dementia and depression is helpful when looking out for early signs of dementia.
Does depression cause dementia?
In studies conducted over the past decade, a strong connection has been made between depression and risk of developing dementia or Alzheimer’s disease. It’s important to note that increased risk is not a cause, but it is a significant association worth paying attention to.
According to this analysis, “6 studies found evidence supporting that late-life depression was associated with a 2 to 5-fold increased risk of dementia.” The same analysis concluded that when it comes to having depression earlier in life, the link seems to be even stronger: “…earlier life or early onset of depression is significantly associated with risk of developing dementia.”
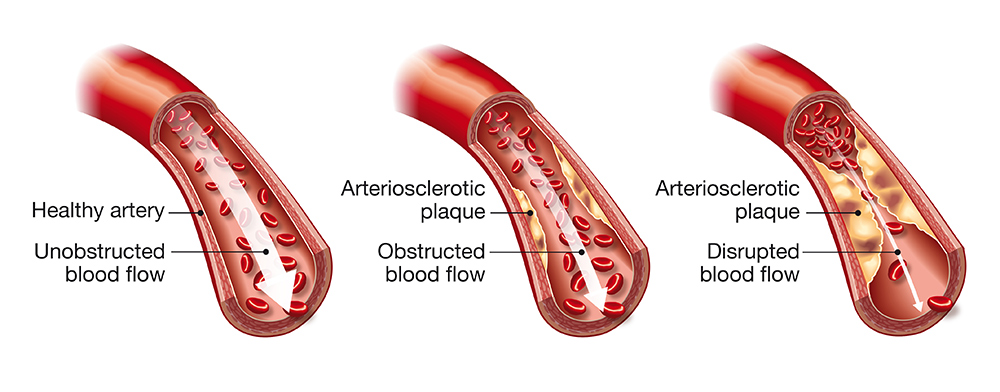
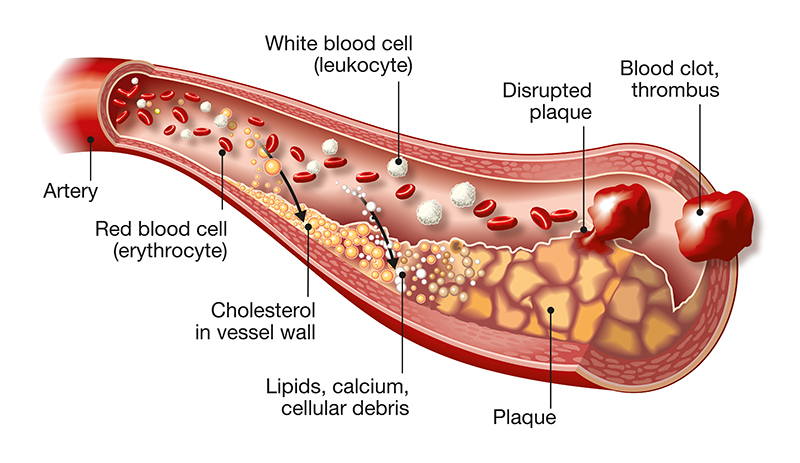
The exact reason for this increased dementia risk due to depression is unknown. It could be that depression changes the brain on a structural level, making it more susceptible to dementia later in life, as this neuropsychologist suggests. Or, as this epidemiologist suggests, the risk increase could be due to reduced blood flow in the brain caused by cardiovascular disease. Cardiovascular disease and depression are often linked.
Whatever it is, enough studies and research have been done to suggest having depression early or later in life can increase your risk for dementia.
How do you know if it’s depression or dementia?
As we mentioned at the beginning of this article, the symptoms of depression and dementia can overlap, making each of them difficult to diagnose in an older adult. But, as the UK Alzheimer’s Association points out, there are key differences between dementia and depression to help you distinguish what is what:
How to treat depression
Because the link between depression and dementia continues to strengthen with research and studies, treating depression in early, mid-, or late life is crucial.
First, if your depression is severe and you are having suicidal thoughts, dial 988. This suicide prevention hotline will connect you with someone who can help.
Most depression is treated either with medication like antidepressants or through alternative routes like talk therapy and cognitive behavioral therapy. Most experts agree that the best results come from a combination of medication and therapy. Medication helps your brain get back to producing a healthy level of serotonin and therapy helps uncover the root issue of your depression so you have longer-term success.
Exercise, a diet of nutrient-dense food and good sleep have also been proven to help those who are suffering from depression.
How to treat depression in someone who has dementia
Treating depression in someone who has dementia can be difficult. Their depression may look different than in someone who does not have cognitive decline, and they may not be able to communicate their symptoms if their disease is progressed, and they are having trouble communicating or feel confused often.
Still, professionals stress that depression in someone with dementia needs to be aggressively treated as depression can worsen the symptoms of dementia.
Depression in someone with dementia can be treated in a similar way as those who have depression but do not have dementia, but the approach should be adjusted based on the dementia-related needs. This study suggests the following treatment strategies for depression in someone who is living with dementia:
Exercise, proper nutrition, sleep and social engagement are always recommended for those who are living with dementia as they can help slow the progression of the disease. These lifestyle habits are especially crucial for those who have dementia and depression. While they aren’t a cure, they promote healthy habits that support blood flow, emotional health and brain health.
If you or a loved one is experiencing symptoms of depression that you suspect could be related to dementia, call your doctor as soon as possible. A medical professional can make a proper diagnosis or point you to someone who can. Depression and dementia are nuanced, separate but also connected illnesses that need to be treated with care. Getting the right diagnosis will ensure you get the care you need.